Topics:
July 26, 2016
For a colonoscopy, the preventative care coverage under the Affordable Care Act means that the doctor is covered. What about the exam center? Is it covered? What about any anesthesia and anesthesiologist? What about the prescription liquid stuff I have to drink before to cleanse my colon? What about the initial visit to the doctor before my procedure?
For most preventive services, only the screening itself is covered at no charge. The actual services required can be subject to cost sharing, and that is based on what plan you have or in many cases, how the doctor’s office bills your insurance.
All ACA-compliant private Major Medical plans (including Marketplace plans) cover the costs for colonoscopy as a screening test, patients may be charged for some services. You may have to pay part of the costs of anesthesia, bowel prep kit, pathology costs, and a facility fee (where the procedure is performed).
Colonoscopies that are done to evaluate specific problems, such as intestinal bleeding or anemia, are usually classified as diagnostic – and not screening – procedures. If that’s the case, you may have to pay any required deductible and copay. The same is true if the colonoscopy was done after a positive stool test (such as the FOBT or FIT) or an abnormal barium enema or colonography. Some insurance plans also consider a colonoscopy diagnostic if something is found (like a polyp) during the procedure that needs to be removed or biopsied.
Before you get a screening colonoscopy, ask your insurance company how much you should expect to pay for the exam. Find out if this amount could change based on findings during the procedure. Learn more at cancer.org.
Rule of Thumb: Preventive care visits are generally covered at no cost if they are evaluating your current health status when you are symptom free. Medical treatment for specific health conditions, on-going care, lab or other tests necessary to manage or treat a medical issue or health condition are considered diagnostic care or treatment, and are NOT considered preventive care.
TIP: In order to get your free annual wellness visit, you have to make sure your doctor codes it correctly. You can generally ask your doctor and insurer what each service will be coded as. This allows you to find out if a service will be billed as preventive care or not.
Updated 7/20/2019:
While the Affordable Care Act includes free preventive procedures like colonoscopies, we’re hearing more and more that people are being asked to pay, from community members. We don’t know anyone who keeps overall records on how big this problem is, but we can tell from this article by being one of our busiest posts.
Under the Affordable Care Act, services recommended by the U.S. Preventive Services Task Force are covered with no out-of-pocket payments. For people between 50 and 75, the task force recommends screening for colorectal cancer using stool testing, sigmoidoscopy or colonoscopy. According to the law, if a polyp is discovered and removed during a screening colonoscopy, there will be no charge, because that’s considered part of a routine colonoscopy.
So: screening colonoscopies are supposed be free if you’re in that age group. Diagnostic colonoscopies (in which the provider is looking for a diagnosis for something like stomach pain) are not free; they’re a “sick person” visit.
More than 15 million colonoscopies are performed annually in the United States. Roughly half of them are screening colonoscopies. How many of those incur some charge? A fair number, anecdotally.
The prices vary widely: We’ve found as little as $600 all in, and as much as $8,000 or even more (see chart at bottom).
There are links to our detailed price lists in this post from clearhealthcosts.com .
Here are examples from our community members’ reporting:
Charge of $3,200; individual paid $370.41: “$3,200 was billed … and $2,331 was the ‘allowed amount’ under my health care plan …. However, I received a separate bill from my doctor who performed the procedure for $800 and the ‘allowed amount’ by my insurance was $370.41 which went to my deductible…. because they found a polyp the procedure coding changed from preventive to diagnostic, therefore, I was no longer covered under preventive care….”
Charge of $8,000; individual paid $800: “I spoke to the CEO of the surgical center. He agreed the fee was high but said there is a standard list of prices that he and most centers adhere to.”
Charge of $2,312; individual paid $844: “Was charged three initial different fees, for MD, facility, and lab work, all reduced … via contract, not payment: (a) 426, reduced to 285; (b) 1400, reduced to 279, and (c) 486 reduced to 280, thus $2312 overall reduced to $844, zero by carrier.”
Charge of $5,104; individual paid $1,650: “I called Kaiser before the procedure to inquire how much it would cost me…. They were vague and would not give me a fixed price, but I was told if there were no special circumstances (in the end, it turned out there were none), it would be around $600 on my plan. Imagine my surprise when I received a bill for $360 for Professional Services, and $1,290 for the hospital bill (my share of each), for a total of $1,650 out-of-pocket. I am on a high-deductible plan, so I paid for 100% of my share.”
Charge of $2,722, insurance paid $743, individual paid $1,979: “I did not ‘shop around’ when I did this. I’m embarrassed to admit that it hadn’t occurred to me to do that. This price check concept is a wonderful service and eye opener for the public. Many thanks.”
We’ve heard a handful of explanations. To be sure, a preventive or screening procedure is supposed to be free, and a diagnostic one (a sick person visit) will not be.
1. For some insurers, we are told, if you had a screening colonoscopy before and you had polyps removed, all subsequent colonoscopies will be considered diagnostic and not preventive. In pretty much every one I’ve heard of, something was removed and tested, so that means the first one is free — and none of the rest are.
So you might expect a screening colonoscopy, and learn only later that the insurance company considers it a diagnostic procedure. The letter to me from my gastroenterologist at right doesn’t suggest there will be a charge — but if I had an insurer who follows this practice, it would be an invitation to a sick-person visit and a hefty bill.
2. Some insurance companies will not cover the facility fee, or will cover only part.
3. We have heard of several cases in which the anesthesiologist was out of network, and billed accordingly. So you might have an in-network doctor who uses an out-of-network anesthesiologist, which you learn of only when you get the bill.
4. Billing confusion: “The most common scenario is when it is billed as diagnostic rather than preventative,” Rebecca Palm, Chief Strategy Officer & Founder of copatient, a consumer healthcare expense management company (www.copatient.com) wrote in an email answer to my question about this. “This can happen if the patient has had a previous test that indicated that a colonoscopy should be performed, or if the patient has symptoms that the provider is trying to diagnose.” She added, “Some providers will also code a colonoscopy as diagnostic if it begins as a preventative screening and, while performing the procedure, they discover and remove a polyp.”
5. That mysterious thing that happens in claims processing. We hear all the time that providers (doctors and hospitals, for example) have to follow different rules for different insurers that may be confusing, or may change.
Palm said: ‘The way that insurers process these codes varies widely. Some insurers require certain coding modifiers to pay the claim as preventative, while others don’t have the capability to distinguish between those codes. If this happens, you can request that the provider code the procedure differently or that the insurer process the claim as preventative based on the coding rules.”
A friend who knows about this process adds: “If there’s a problem & it’s not clear, it has to be processed as diagnostic & not preventive. I’ve fought claims on that for people even on something that wasn’t straightforward, something like the doctors wanting additional images or views or unclear pictures because of dense tissue in the body made them less than clear; where an immediate problem isn’t exactly found & all of it has to be considered diagnostic still.”
So yes, the coding part is mind-numbing. If you don’t believe us, look at this article on the subtleties of coding.
The Affordable Care Act is not the cause of this; it’s the product of unintended consequences.
Preventive screenings (including colonoscopies) were made free under the A.C.A. Providers of such screenings, of course, saw an opportunity for increased business. These screenings are suddenly quite heavily marketed (see my gastroenterologist’s letter above).
The problem of surprise out-of-network bills is not a new one, of course. One study estimated that 40 percent of out-of-network bills came as a surprise.
As we always say, know before you go. As a preliminary step, know what’s in your insurance plan.
First, make sure it’s a preventive (screening) colonoscopy. If it’s not preventive (screening) but rather a diagnostic colonoscopy — looking for a diagnosis for a symptom in your GI tract, then it can be charged as a “sick person” visit — just as a screening mammogram is covered under preventive care with A.C.A.-compliant plans, but a diagnostic one is not.
Questions to ask:
Take notes, and take names and phone numbers. If you need to question a bill later, it’ll be much easier.
Hospitals and other facilities do not police this as carefully as they might in many cases, and after the fact — even with a huge argument — it’s not always possible to get covered. Many insurers will take the position that it’s your fault, even if you did everything you could to protect yourself. But your case will be stronger if you ask up front, get commitments and assurances in writing, and take names and phone numbers.
Also, we don’t give medical advice, but our friends over at the American Board of Internal Medicine Foundation do, via their Choosing Wisely campaign. Here is a fact sheet on colonoscopies from them.
No, you cannot be charged for a pre-colonoscopy consultation after a screening colonoscopy.
No, you cannot be charged for any lab tests after a screening colonoscopy.
Other resources: Here’s a National Women’s Law Center fact sheet on what to do if you think you’re being charged when you shouldn’t be.
Here’s a Kaiser Family Foundation paper with a set of scenarios for coverage, dating to 2012 (some clarifications have been issued since then, but this is pretty thorough).
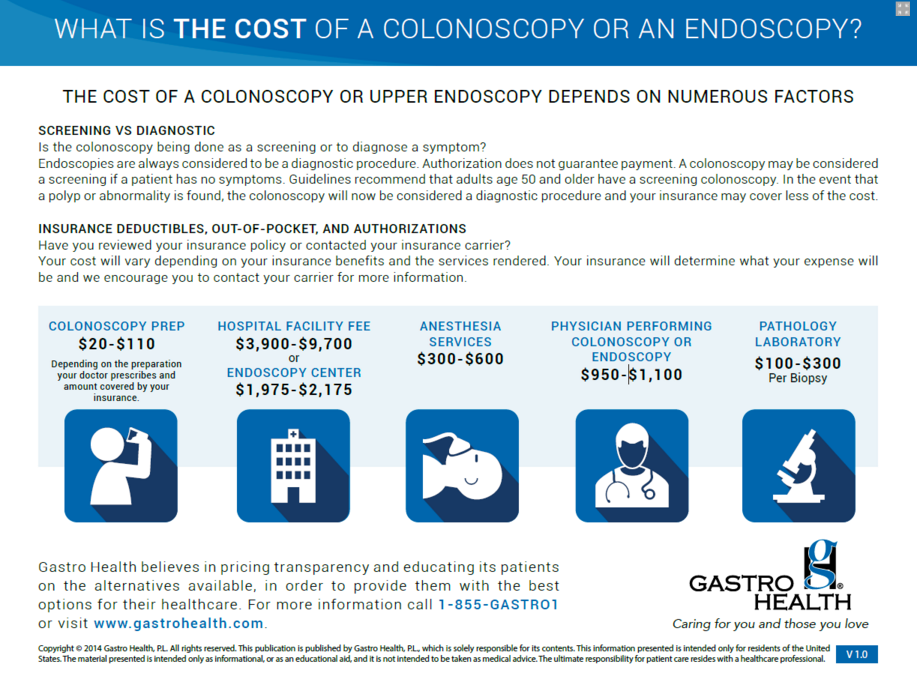
And finally, here’s a sheet from a provider listing the range of prices. While the facility fee is scary ($1,975 to $9,700? come on!), we also want to point out the fee for the “prep” stuff: Here’s a blog post about a person who found out that the cost could be $12.11 without his insurance, or $38 with. I guess he should feel lucky that he wasn’t charged $110.
We’d be happy to have your join our team of independent agents.
JOIN NOW